The vital role of vascular access nurses in reducing infection risk

By Medline Newsroom Staff | September 11, 2023
The spring 2023 Leapfrog Hospital Safety Grade data highlighted ongoing high central line-associated bloodstream (CLABSI) infection rates due to a pandemic-related decline in infection management protocols and priorities.
Vascular access nurses, responsible for inserting PICC lines, play a key role in helping reduce the risk of CLABSIs. They are highly trained, certified, and know first-hand the impact infection can have on patients and families.
In recognition of Vascular Nurses Week, the Medline Newsroom spoke with vascular access nurses from renowned healthcare organizations, including The University of Kansas Health System, Children’s Mercy Kansas City, and Norman Regional Health System, to discuss their critical role in healthcare, and the importance of training and internal team collaboration to optimize outcomes and care.
The value of evidence-based, hands-on training
According to the Centers for Disease Control and Prevention, up to 70% of CLABSIs can be prevented by implementing evidence-based strategies.
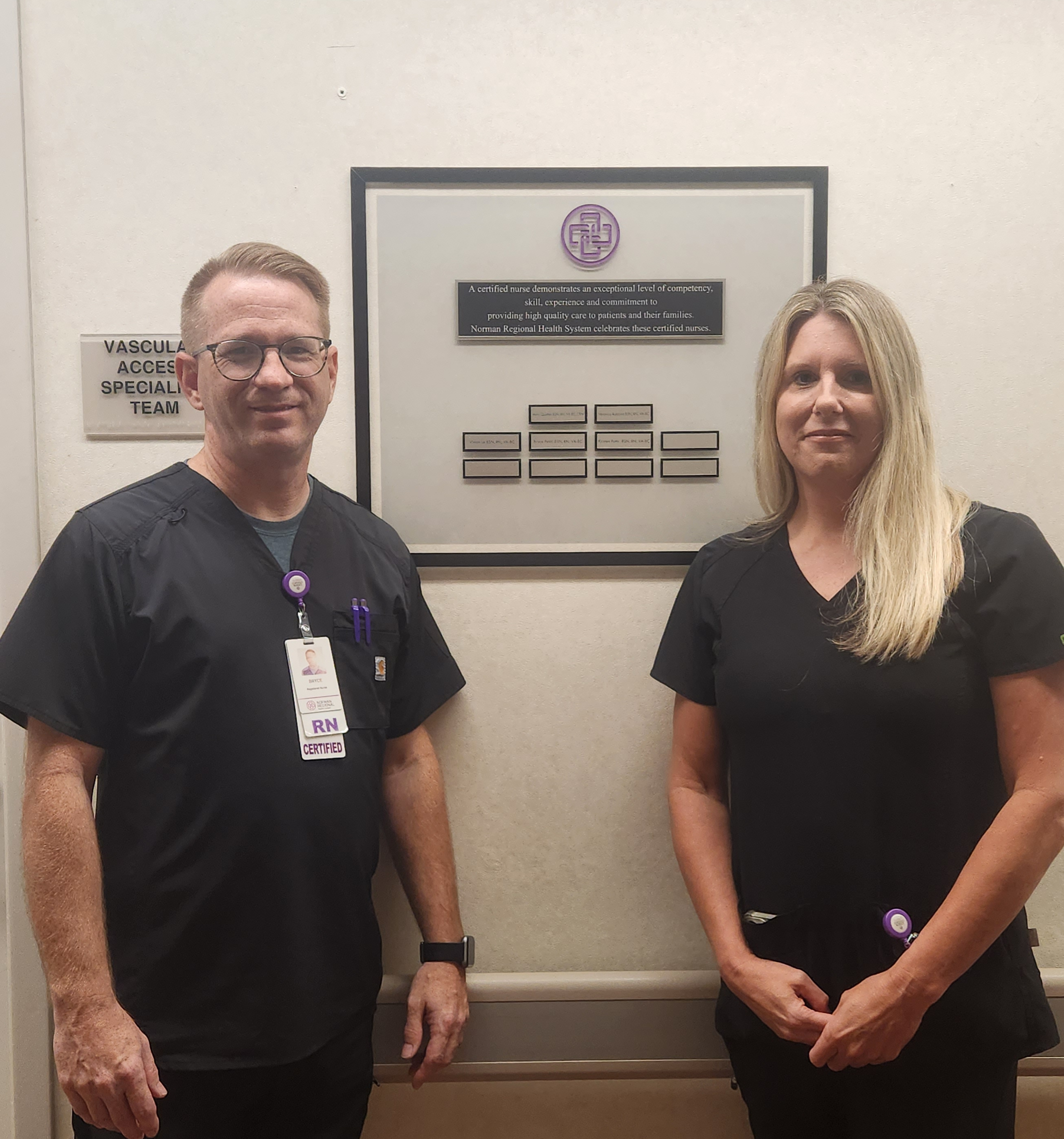
Bryce Petitt and Veronica Robbins, Norman Regional Health vascular access nurses
Bryce Petitt at Norman Regional Health System has been a vascular access nurse for more than 20 years and now handles onboarding and education for team members. While technological advances such as ultrasounds, X-rays and electrocardiograms (ECG) continue to aid in determining the best device and accurate placement, “back to basics” education is still important for building and maintaining important skill sets.
“Vascular access is a growing part of healthcare and sometimes frontline caregivers may not have time or the knowledge base to think about what device the patient is receiving or how long the IV will last,” said Petitt. “Our knowledge is a valuable asset to the teams around us. I encourage vascular access nurses to stay up-to-date on fundamental practices, including what a central line is, what a PICC line is, how to maintain lines, how to properly keep dressings on, and the importance of maintenance for flushing.”
For Emily Evans, RN, vascular access team education and quality improvement coordinator at Children’s Mercy Kansas City, “moment in time” observation is important for process improvement. She prioritizes bedside time with vascular access nurses to help determine education priorities for her team.
“When a nurse puts in a consult to vascular access, it is important that we look at the whole patient to assess which device would work best for them.”
Dustin Broyles
Vascular Access Nurse, The University of Kansas Health System
“I’ve always enjoyed providing direct patient care,” said Evans. “As a member of our leadership team, I would never expect my coworkers to do something I am not comfortable or well-versed in. Being hands-on, working side-by-side with my vascular access nurses helps me connect on a personal level and allows us to tackle or troubleshoot challenging cases together. Working alongside them helps me get their direct input on the type of education or quality improvement projects they’d like to see.”
Evans shared that a staff-driven education request focused on how to place femoral and axillary PICC lines. The vascular access team collaborated with Interventional Radiology and the ICN to standardize the process and education of placing these lines.
Improving collaboration to optimize care
While there are prescribed instructions for insertions, close collaboration with a patient’s nurse, physician and other team members, allows vascular access nurses to demonstrate their expertise, while ensuring holistic patient care.
“Our line of work can provoke a lot of anxiety from patients,” said Dustin Broyles, a vascular access nurse with The University of Kansas Health System. “It can be a scary experience and patients may have been traumatized by being stuck multiple times. When a nurse puts in a consult to vascular access, it is important that we look at the whole patient to assess which device would work best for them. Sometimes, this can be a tough conversation to have with nurses and physicians, leading to misunderstanding and a breakdown in collaboration.”

The vascular access team at Children’s Mercy Kansas City
Petitt says that “vascular access nursing is multi-faceted. It can be procedural—do our prescribed order and leave the patient’s room—but can also provide consultation to interpret the best vascular access device for the patient. There can be a lot of autonomy to do what’s best for the patient, but I have found it crucial to be able to successfully collaborate with various practice areas, including infection prevention, pharmacy and nursing.”
Broyles shared that shadowing opportunities – for internal medicine students and other team members – can help improve the overall understanding of the role and value of a vascular access nurse.
When thinking about collaboration, Evans advises, “Successful collaboration across multiple disciplines can be challenging especially when it’s busy, but it’s imperative to share our specialized vascular access knowledge to aid in decision making. Just remember, we’re all in it for the same reason and that is to do what’s best for patients.”
Medline is committed to helping vascular access team enhance clinical practice to deliver high quality patient care. Learn how Medline is supporting vascular access through products, best practice guidance, and education and training.
Medline Newsroom Staff
Medline Newsroom Staff
Medline's newsroom staff researches and reports on the latest news and trends in healthcare.
