Post-Acute Care: 3 Action Items to Prepare for the 5-Star Rating Unfreeze
By Medline Newsroom Staff | April 24, 2019
This is a guest column by Ellen Kuebrich, Chief Strategy Officer of Providigm.
Spring is here, and everything is thawing… including Health Inspection Star Ratings. Here’s a quick primer on how the unfreezing affects post-acute care facilities and how administrators and clinicians can prepare for “the great thaw.”
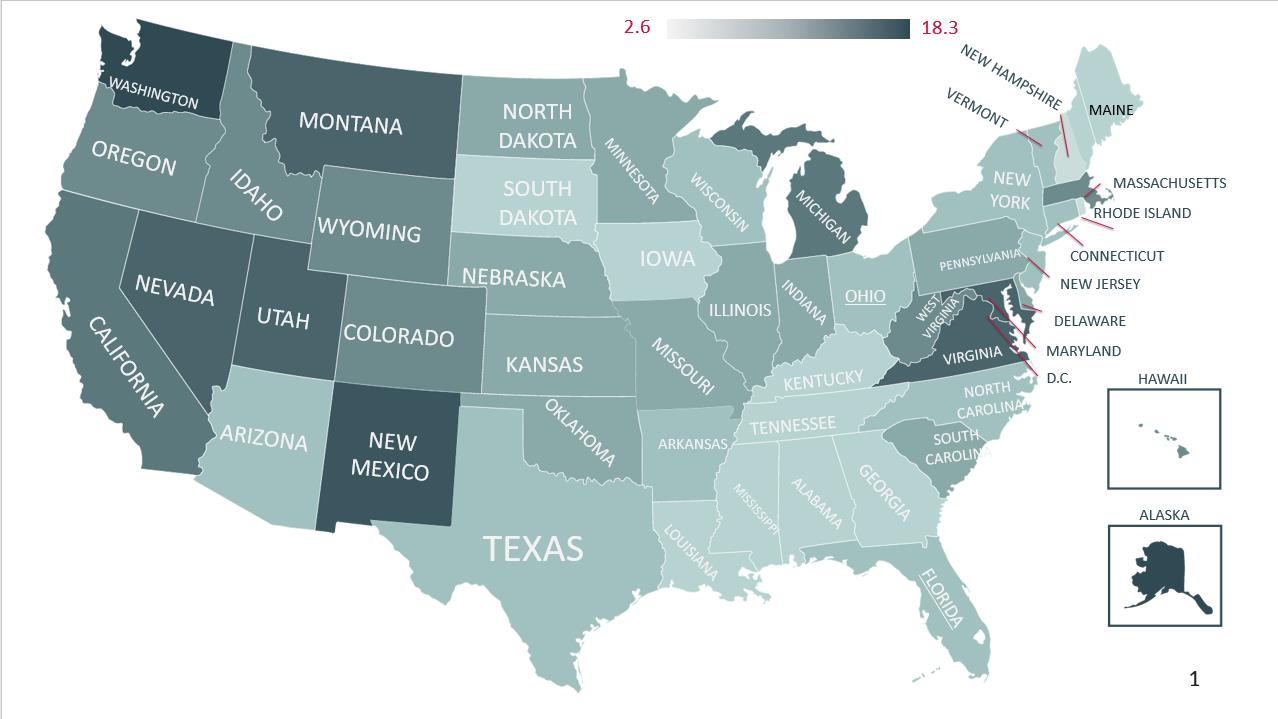
In April, the Centers for Medicare and Medicaid Services (CMS) will resume calculating health inspection scores by using a facility’s three most recent surveys, with the most recent carrying the greatest weight. For many facilities, the most recent survey was their first experience with the new Long-Term Care Survey Process (LTCSP). The LTCSP has had varied results across the US, with average deficiencies per survey ranging from as low as 2.6 to as high as 18.3 depending on the state (see graphic). As CMS evaluates the LTCSP, these averages should start to even out, but as these most recent surveys will impact your ‘unfrozen’ health inspection rating, it’s important to understand how these averages will affect your calculation.
Five-star ratings are scored on a bell curve, based on state averages. So, for example, if the average number of deficiencies in a state was three, then even a facility receiving only three deficiencies (which by most standards is very good) would likely fall into the three-star, or average, range for their health inspection rating. On a recent webinar, the American Health Care Association estimated that one third of facilities would experience a drop of at least one star in their overall rating, with half of facilities staying the same, and the remainder improving.
How to Prepare
Here are a few concrete steps operators can take to support five-star ratings:
- Prepare staff for this year’s survey by using the available LTCSP process.
- Look at the other two domains of five-star. There are now elevated standards around staffing levels and Patient Driven Payment Model (PDPM) measures.
- Now is the time to ensure you are ready for Phase 3 of the Final Rule. Execute the Quality Assurance and Performance Improvement (QAPI) program described in your QAPI plan, review and amend existing Compliance and Ethics policies, as necessary, and ensure that you have a dynamic Competency program in place.
Learn how Medline helps long term care facilities reduce costs, increase quality outcomes and drive revenue.
Medline Newsroom Staff
Medline Newsroom Staff
Medline's newsroom staff researches and reports on the latest news and trends in healthcare.