Leading a hospital through change during COVID-19

Illinois healthcare worker honored for her role in developing mobile site to test and triage patients
By Medline Newsroom Staff | July 28, 2020
Illinois reported its first COVID-19 case on January 23, 2020. More than six months later, government, healthcare providers and community members continue to remain vigilant when it comes to keeping communities safe.
“When we first started to hear about COVID-19, I initially thought about how it would impact us,” says Kathryn Martinez, executive vice president, chief operating officer and chief nursing officer at Illinois-based FHN. “Will being in a rural community help keep us secure from seeing a rush of cases?”
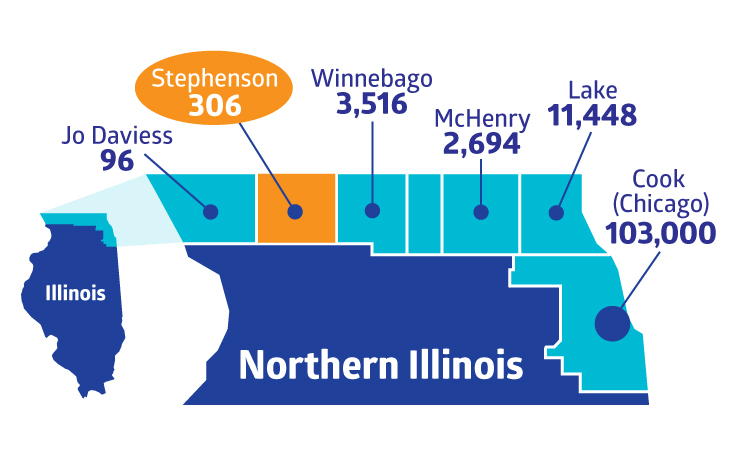
Breakdown of COVID-19 cases in Northern Illinois counties according to the Illinois Department of Public Health. FHN in Stephenson County has remained vigilant and proactive in order to protect its community and provide safe care to patients.
Before cases started appearing in northwest Illinois, FHN began developing a proactive plan to effectively – and safely – care for COVID-19 patients.
“We are an independent organization, so we don’t necessarily have all the resources available to us that some of the large hospitals do,” Martinez shared.
As the organization worked to set up mobile testing and its alternative care site to triage potential COVID-19 patients, they needed a team member who could help train the nearly 100-staff members working in the tent.
Passion, protocols and personality
For Katie Alvarado, FHN’s director of imaging, healthcare intrigued her even as a child.
“My uncle owns a portable x-ray service, which helped propel my interest in imaging, but I also endured my own health difficulties. I would pass out for unknown reasons when I was young. Seeing how dedicated my doctors were to finding a cause really motivated me to pursue the field.”
Today, she is a leader of 50-plus team members at FHN Memorial Hospital. Her positive attitude, strategic vision and innate ability to help inspire added another project to her plate after being handpicked to develop the protocols for the COVID-19 alternative care and mobile testing sites. Part of the responsibility? Successfully training 100 staff members during an unprecedented pandemic.
“Our first step was to research and try to determine best practice. We leveraged third-party sources and our valuable panel of nursing and provider experts at FHN,” Alvarado shared. “From this, FHN developed a protocol to treat mild and moderate COVID patients in the patient aid tent. If someone required a level of care we couldn’t provide in the tent, we needed to figure out how to transfer the individual safely into the emergency department. Lots of cross-department collaboration went into determining best protocols for serving our patients.”
According to Alvarado, FHN saw approximately 50 patients per day for testing or appointments in the tent when capacity spiked since being operational.
“The alternative care site allowed the emergency room to concentrate on patients who truly needed emergency care. We have not had to worry about when a heart attack victim or a stroke victim comes in or having to allocate resources to patients who may not have necessarily needed emergency room care. Because of this, we can give our patients and our community members the right care at the right time, and at the right place,” added Martinez.
Katie’s dedication to getting the tent up and running and her natural ability to lead team members through change is why her CNO nominated for her the Medline “Works of Heart” program.
Know a deserving healthcare worker? Nominate them for the “Works of Heart” program.
Medline Newsroom Staff
Medline Newsroom Staff
Medline's newsroom staff researches and reports on the latest news and trends in healthcare.
